Communication Orders After Discharge
In 2019 and 2020, Bellin Health documented four serious patient safety events that were attributable to gaps at discharge. A review of two years of data on patient safety events demonstrated that the highest frequency of errors was attributable to diagnostic tests not being ordered or performed. Inpatient and/or discharging providers are not the correct resource for follow-up because they could be out of rotation and not be back for an extended period and, therefore, would not see the patient’s test results. This project was picked as a quality improvement priority as there exists a process gap to communicate recommended labs or imaging at discharge (in a standard fashion) to the appropriate managing provider performing follow-up with the patient, leaving the opportunity for delays in patient care. Patients with delays in care or treatment are more likely to have readmissions and preventable adverse events.
AIM: By September 2021, develop a system-wide process to communicate diagnostic test follow-up orders needed post-discharge, targeting zero harm in related post-discharge diagnostic test safety events and closure of communication order within three days. Metrics and associated targets for the project included the following:
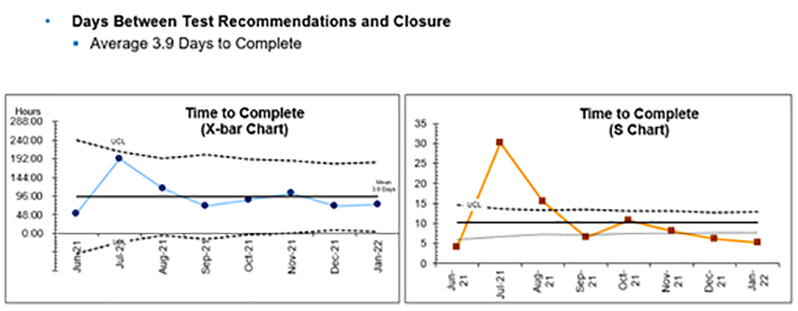
- Time Between Recommended Orders and Closure (target three days or less)
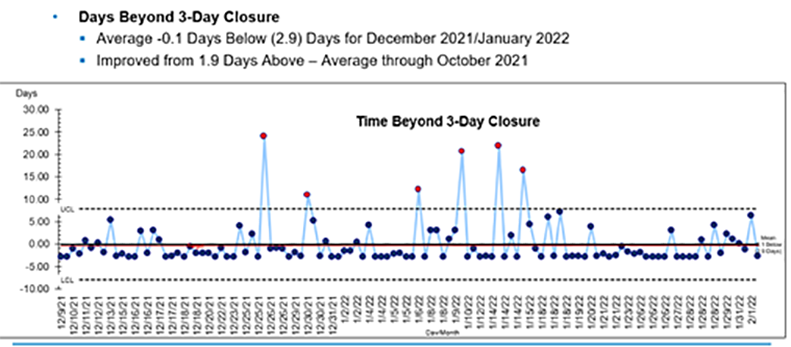
- Closure of Recommended Labs/Imaging Beyond Three Days (target < one day above)
- Patient Harm Events Related to Discharge Diagnostics (target = 0)
- Recommended Lab and Imaging Communication Order in Discharge Summary (target 98%)
- Volume of Hospitalist-Placed Outpatient Lab/Imaging Orders (target = 0).
We set out to develop a process with our hospitalist group with the end goal of spreading the process system-wide.
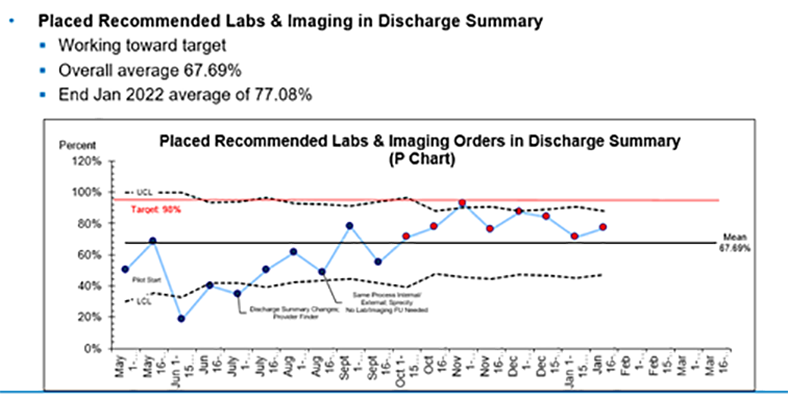
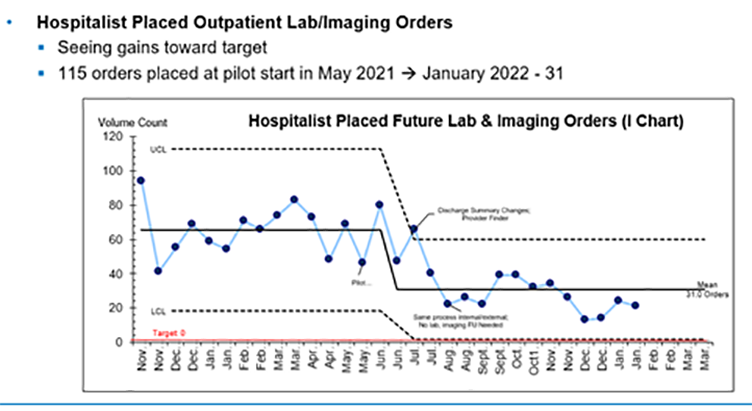
We implemented this process, borrowed from UW Health, making adjustments with Plan-Do-Study-Act (PDSA) findings. The general concept is that we started a pilot with our hospitalist group where providers are able to document recommended lab and imaging post-discharge in a communication order. When utilizing the discharge order set, the hospitalists must choose the recommended labs/imaging order and complete details or select that no labs or imaging are needed post-discharge. This communication order goes to the selected provider in-basket for Bellin-internal providers. Non-Bellin providers will also see the recommended labs/imaging post-discharge in the discharge summary (as long as all orders are pulled into the discharge summary). Upon receiving the order in a specific “order requests” in-basket, Bellin-internal providers review the recommendations and place orders or adjust the plan of care per their medical expertise. Non-Bellin internal providers receive recommendations in the discharge summary and follow their established process to complete needed follow-up. See high-level change pre- and post-implementation.
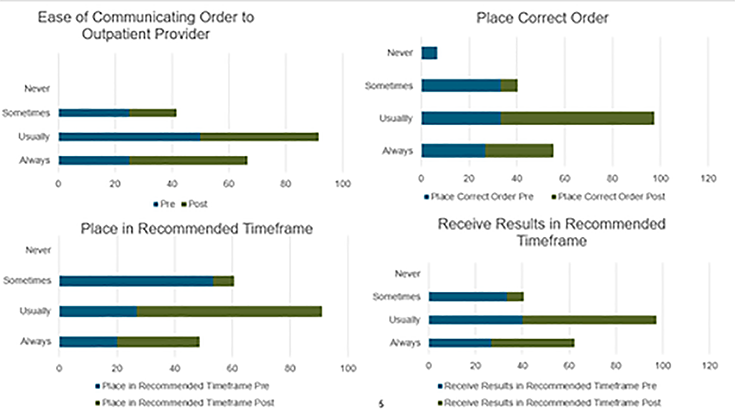
We have had zero patient harm events related to discharge diagnostic needs since prior to the pilot start. This project’s spread and process control were impacted by the pandemic. While averages show improvement, we do see data points above the upper control limit and will need to continue investigations on those outlier data points and determine what actions are needed to sustain work closer to targets. Our next goal remains to spread into the emergency department, which was delayed due to surge volume.