Transitional Care Management: An Evidence Based Approach to Eliminating Care Gaps
In recent years, Upland Hills Health (UHH) restructured to a hospitalist model, expanded its service area to include seven primary care clinics and converted all patient care areas to a shared electronic medical record (EMR) solution. Despite significant growth and improvements over a short amount of time, continuity of care remained challenging, especially for patients hospitalized with congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD) and diabetes. There was an innate need for a more collaborative approach to coordinating care and an even greater need to increase communication with primary providers after a hospital stay. To improve the patient experience and quality outcomes and to reduce readmission rates, UHH saw the implementation of transitional care management (TCM) as a prime opportunity to bridge the gap between the inpatient and outpatient worlds.
TCM provides care coordination for 30 days following hospitalization and is designed to eliminate gaps in care and reduce readmission rates. It ensures a comprehensive discharge plan, prompt follow-up communication to patients and/or caregivers, complete medication reconciliation, timely follow-up with a primary provider and referrals to community resources. TCM has been recognized since 2013 by the Centers for Medicare & Medicaid Services and many insurers as a reimbursable, preventative wellness program. UHH applied for and was awarded grant funding from the Federal Office of Rural Health Policy to incorporate this best practice to its everyday workflows. With financial support totaling $538,987 over a three-year period, UHH was set to begin development of a TCM program in the fall 2019. Looking back, some may think that taking on a sizable quality improvement (QI) project at the onset of a pandemic was just plain crazy, but there was no greater time to ensure care coordination.
Year one of the project emphasized the development of a strong foundation. Hiring qualified staff, establishing measurable goals and creating action plans were initial priorities. A day-long Kaizen event in December 2019 proved to be a crucial element. More than 25 UHH staff members and two facilitators from the Rural Wisconsin Health Cooperative focused on continuous improvement cycles, analyzed current processes, identified areas of breakdown and developed new workflows to optimize communication and standardize work. A plan-do-study-act model was used to implement plans for small tests of change, and a TCM leadership team began meeting regularly to oversee project progress and meet grant deliverables.
An initial target population consisted of adult patients with a diagnosis of CHF, COPD or diabetes who were hospitalized at UHH and would receive follow-up care at a UHH primary care clinic. These chronic conditions paired with other co-morbidities, problem-prone medications and increased social isolation during a pandemic set up the perfect storm to put patients at an increased risk of complications and readmission. TCM nurses based in the hospital prioritized attending interdisciplinary rounds to anticipate discharge plans and potential needs of patients returning home. Standardized processes guaranteed that patients were called within two business days of discharge. Use of templates and message routing within a shared EMR provided complete, real-time updates to primary providers. Appointment blocks in clinic schedules helped to consistently provide a focused follow up visit within a specific timeframe. A comprehensive spreadsheet shared by TCM nurses, coders, billers and data analysts was used to track the necessary components for reimbursement during the 30 days after the hospitalization.
Patient education and engagement were identified as vital components of the QI project. TCM nurses partnered with patients to provide the tools and information they needed. Organizationally, a decision was made to use materials from two approved sources. Additionally, zone tools for CHF, COPD and diabetes were utilized. These visual references, resembling a stop light, helped patients to more easily recognize warning signs and manage symptoms. To increase patient engagement, grant funds were used to provide patients in need with scales, medication planners, blood pressure monitors and pulse oximeters. The cost of transportation to medical appointments was also covered for those in need to ensure access to follow up with providers and specialists. For patients at high risk of readmission, TCM nurses provided additional follow-up phone calls over the course of 30 days following the hospitalization to educate on self-management and increase patient engagement.
By year-two of the project, TCM was extended to all patients hospitalized at UHH who would receive follow-up at a UHH primary care clinic, regardless of age or diagnosis. Despite the increased patient volumes, it seemed there was still a significant number of patients being missed—those following up in a UHH primary care clinic after being hospitalized elsewhere. This included patients transferred from UHH to a higher level of care as well as those admitted directly to other hospitals. With the development of reports within our EMR and collaboration with health information technology staff at other area hospitals, automatic notification processes were established. This allowed continuity of care for UHH patients even when they hospitalized elsewhere. This outreach alone nearly doubled the number of patients served by TCM within two years of implementation.
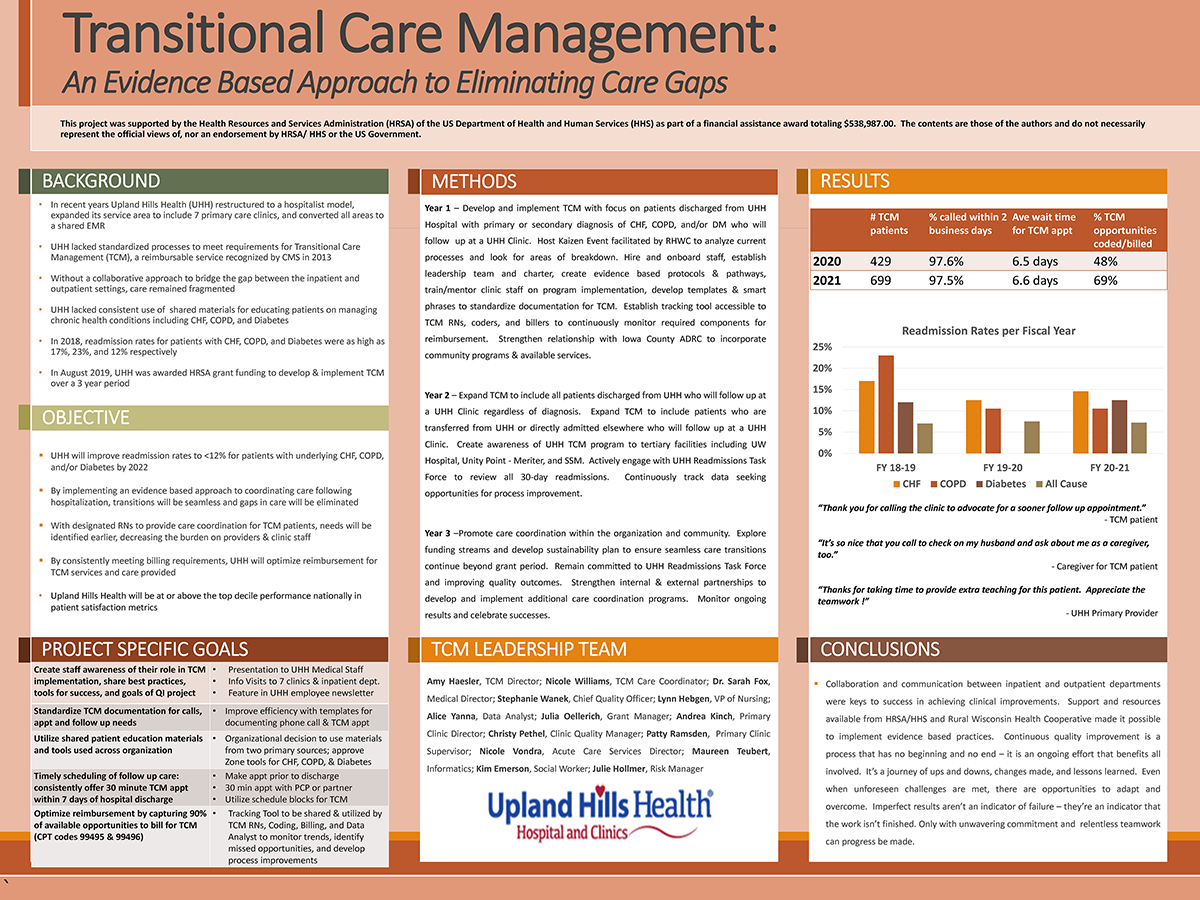
Now in its third and final year of grant funding, UHH is focused on sustainability. Implementing a QI initiative during a pandemic had its challenges, but it has certainly been beneficial for patients as well as providers. Through follow-up phone calls alone, TCM nurses have made numerous good catches related to medications being taken incorrectly, referrals that had gone amiss or a need for increased services in the home. Standardized processes and streamlined documentation have resulted in increased reimbursement for TCM. Missed opportunities are tracked and reviewed on a monthly basis for continued improvement. Consistently, more than 97% of all discharged patients receive a follow up call within two business days, and on average, patients are seen within seven days for a TCM appointment. Primary providers have expressed appreciation for the increased coordination and patient education being completed.
Optimization strategies to reduce 30-day readmission rates continue at full strength. Despite efforts made during the period of grant funding for this project, these rates remain higher than desirable, especially for patients with CHF, COPD and diabetes. When reflecting on the impact of recent challenges, we are soon reminded of the abrupt shut down of services and limited availability of community resources in 2020-2021. This included cancelled outpatient services, routine well-visits in our clinics, transportation agencies and supportive home care programs. The overall risk of readmission for anyone with chronic conditions quickly increased; yet, outlets for assistance seemed more limited than ever. TCM nurses were able to provide weekly calls to those at highest risk to help manage symptoms at home. A multidisciplinary readmission taskforce was established to review all unplanned 30-day readmissions. This group continues to meet bi-weekly to identify root causes and opportunities for improvement.
In conclusion, collaboration and communication between inpatient and outpatient departments is the key to success in achieving clinical improvements. Patient-centered care isn’t a singlehanded effort; rather, it is a continual effort by all members of our organization. It requires a culture of quality and a mutual understanding of best practices and evidence-based care. Continuous improvement is a process that has no beginning and no end—it is an ongoing effort that benefits all involved. It’s a journey of ups and downs, changes made and lessons learned. Imperfect results aren’t an indication of failure—they’re an indicator that the work isn’t finished. Even when unforeseen challenges are met, there are opportunities to adapt and overcome. Only with unwavering commitment and relentless teamwork can progress be made.
(This project was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) as part of a financial assistance award totaling $538,987.00. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by HRSA/HHS or the U.S. government.)
 Upland Hills Health's quality improvement dashboard 2022
Upland Hills Health's quality improvement dashboard 2022