Aspirus Stevens Point Hospital, Stevens Point, 2025 Quality
Improving Mortality Index
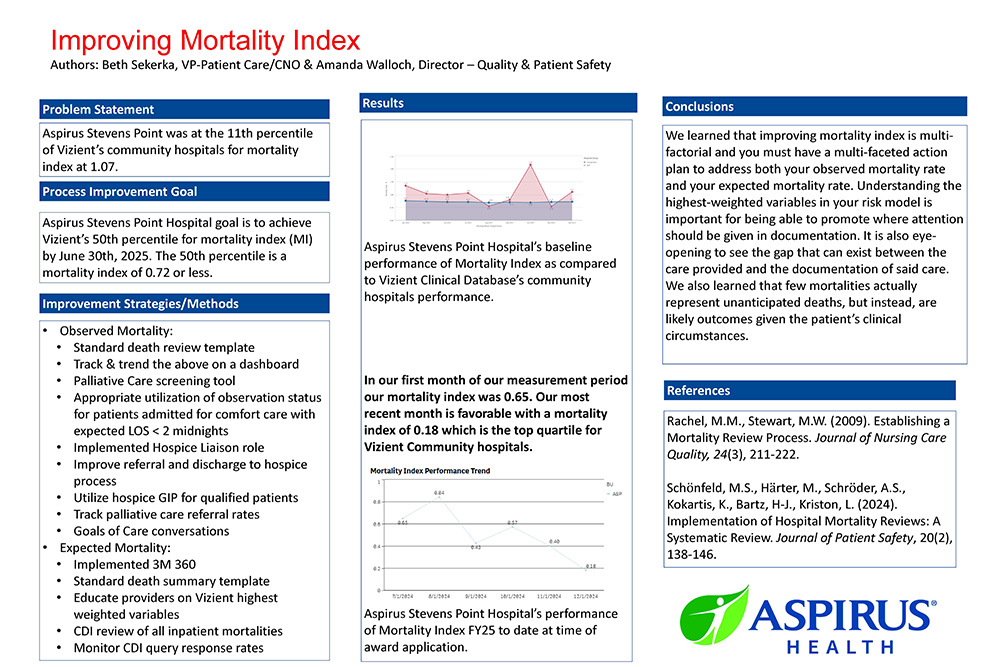
Aspirus Stevens Point Hospital’s goal was to achieve Vizient’s 50th percentile of community hospitals for mortality index by June 30, 2025. The 50th percentile is a mortality index of 0.72 or less. To improve the mortality index you must improve both your observed mortality rate and your expected mortality rate.
To improve our observed mortality rate, a review tool was implemented to track and trend themes and opportunities in inpatient mortality. An inpatient palliative care screening tool was developed and trialed. Appropriate observation utilization was also considered for patients being directly admitted into comfort cares with the expected length of stay of less than two midnights. The team partnered with the hospice team to implement a hospice liaison role. This role was sourced to counsel patients, both in the emergency department and inpatient units, regarding end-of-life options. They team up with providers and clinical staff to provide hospice consults and assist with transitioning patients into hospice after discharge or hospice GIP when appropriate. They participate in multi-disciplinary rounds to assist with identifying patients who may be hospice eligible.
To improve the expected mortality rate, Aspirus implemented 3M’s 360 product to assist with identifying coding opportunities via artificial intelligence. Vizient’s risk models were studied to determine the highest weighted variables. The clinical documentation improvement team queries provide as appropriate to capture these variables. A standard death summary template was developed to assist with documenting the patient’s clinical status to aid coding with capturing higher weighted variables. The team learned that improving mortality index is multi-factorial and must have a multi-faceted action plan to address both observed mortality rate and expected mortality rate. Understanding the highest-weighted variables in the risk model is important for being able to promote where attention should be given in documentation. It is also eye-opening to see the gap that can exist between the care provided and the documentation of said care. They learned that few mortalities represent unanticipated deaths, but instead, they are likely outcomes given the patient’s clinical circumstances.
To improve our observed mortality rate, a review tool was implemented to track and trend themes and opportunities in inpatient mortality. An inpatient palliative care screening tool was developed and trialed. Appropriate observation utilization was also considered for patients being directly admitted into comfort cares with the expected length of stay of less than two midnights. The team partnered with the hospice team to implement a hospice liaison role. This role was sourced to counsel patients, both in the emergency department and inpatient units, regarding end-of-life options. They team up with providers and clinical staff to provide hospice consults and assist with transitioning patients into hospice after discharge or hospice GIP when appropriate. They participate in multi-disciplinary rounds to assist with identifying patients who may be hospice eligible.
To improve the expected mortality rate, Aspirus implemented 3M’s 360 product to assist with identifying coding opportunities via artificial intelligence. Vizient’s risk models were studied to determine the highest weighted variables. The clinical documentation improvement team queries provide as appropriate to capture these variables. A standard death summary template was developed to assist with documenting the patient’s clinical status to aid coding with capturing higher weighted variables. The team learned that improving mortality index is multi-factorial and must have a multi-faceted action plan to address both observed mortality rate and expected mortality rate. Understanding the highest-weighted variables in the risk model is important for being able to promote where attention should be given in documentation. It is also eye-opening to see the gap that can exist between the care provided and the documentation of said care. They learned that few mortalities represent unanticipated deaths, but instead, they are likely outcomes given the patient’s clinical circumstances.