Vol. 66, Issue 50
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Click here to view past issues
IN THIS ISSUE
- Registration Now Open for WHA 2023 Physician Leadership Development Conference
- Tell Your Story in the 2023 Wisconsin Health Care Workforce Report: Submit Stories by Jan. 16, 2023
- At Final Hearing, Legislative Council Study Committee on Occupational Licenses Advances WHA-Backed Legislation to Improve Health Care Licensure Process
- Advocate Health’s Nan Gardetto Receives WHA Trustee Award
- Board Members Emphasize Workforce Concerns, Discuss Financial Pressures on Panel in Milwaukee
- WHA Awarded AHW Seed Grant for Community-Based Initiative
- Congress Poised to Pass One-Week CR Extension, Including Funding for MDH and LVH Hospital Designations
- GUEST COLUMN: Health Care Staffing Shortages Make Big Impact on Liability and Workers’ Compensation Risks
- Webinar Recap: What’s Your Antibiotic Stewardship New Year’s Resolution?
- Social Care - Beyond Resources Webinar Recap
EDUCATION EVENTS
Jan. 6, 2026
Age-Friendly Webinar Series Featuring Advocate HealthJan. 14, 2026
Caring for Wisconsin’s Caregivers Well-Being First Champion Challenge for Credentialing KickoffJan. 28, 2026
2026 WHA Health Care Leadership AcademyClick here to view education event calendar
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Thursday, December 15, 2022
Board Members Emphasize Workforce Concerns, Discuss Financial Pressures on Panel in Milwaukee
WHA board members participated as key speakers for the Wisconsin Health News (WHN) event on Dec. 13 held in Milwaukee. The panelists featured Cathy Jacobson, CEO, Froedtert Health; Peggy Troy, CEO, Children’s Wisconsin; and Dr. Sue Turney, CEO, Marshfield Clinic Health System. The panelists discussed top issues impacting their hospitals, including capacity and delayed discharge concerns and financial challenges, but all three health system leaders emphasized workforce as a main pressure point.

From left: WHN Editor Tim Stumm, Susan Turney, Cathy Jacobson, Peggy Troy
When asked what the biggest issue facing hospitals is right now, Jacobson replied simply “workforce, workforce, workforce.” She went on to explain that includes workforce shortages, the cost of workforce, and the inability to do anything about it.
“A lot of people in different industries are experiencing workforce shortages, but our workforce issues are different,” said Jacobson. “First of all, this workforce is battered and bruised from COVID. And second, other businesses have the ability to shut their doors when they don’t have workers, but we cannot do that. Our emergency rooms remain open 24/7,” she continued.
Turney agreed and elaborated on the scope of the health care workforce shortage. “Pre-pandemic, our workforce was already in crisis. We were already having difficulty with recruiting and retaining health care workers,” said Turney. “But it’s not just clinicians, but all positions within our facilities,” Turney added.
Troy added that remedying the problem will take time and maintaining the workforce pipeline, for all types of positions, is a tactic they are using for the long term. “It takes a long time to train a nurse, but we have other opportunities, too,” Troy said. “We need to teach younger kids about what health care is all about and the many different avenues in which they can work in a hospital.”
When it comes to financial pressures, Jacobson said while inflation is a factor, she called out utilization as the main driver. She explained there are two things happening – patients coming into the hospital are sicker, and patients are boarded in the hospital who do not need to be due to inadequate discharge placement. Both of these require more staff and more resources, adding to the cost of care.
Jacobson said, “This is clearly exacerbating all the issues we are having right now. We are working with our colleagues from the Wisconsin Hospital Association to try to get money to the right parts of the system to open up capacity in the hospital.”
Troy added that emergency department visits at Children’s Wisconsin have tripled this year as they are dealing with a “tripledemic,” with a high volume of cases with respiratory illnesses, like RSV, flu and COVID. Turney shared that Marshfield Clinic has stood up their incident command to manage capacity issues.
“Beds are full, and we don’t have the staff. That means patients are sitting in emergency rooms and not getting the care they need,” Turney said.
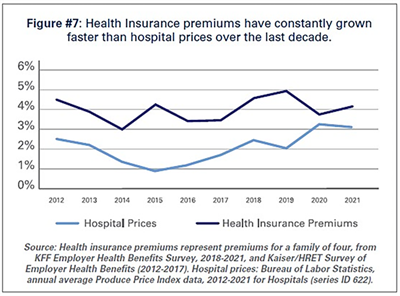 Both Turney and Jacobson noted a disconnect between what consumers pay in insurance premiums and what insurance companies pay hospitals for health care. As an American Hospital Association (AHA) report points out, hospital prices have grown an average 2.1% per year over the last decade, about half the average annual increase in health insurance premiums.
Both Turney and Jacobson noted a disconnect between what consumers pay in insurance premiums and what insurance companies pay hospitals for health care. As an American Hospital Association (AHA) report points out, hospital prices have grown an average 2.1% per year over the last decade, about half the average annual increase in health insurance premiums.
“We haven’t raised our prices. If you are getting a double digital increase from your insurance company, that is not coming to your local hospital,” Jacobson said.
All three panelists agreed that changes are needed to address these problems, and they called on the state to help with investments in the health care workforce and easing regulatory barriers.
“We are not looking for a bailout. We need some help on the topline, like with retention bonus. The state can help us with that. Also, it should not take months to get someone credentialed and licensed to work in Wisconsin,” said Jacobson.
Troy emphasized the importance of addressing social determinants of health to help alleviate the high acuity of patients. Jacobson expressed concern for funding social determinants of health initiatives as hospital margins tighten and suggested partnering with the community in this space.
“When we don’t have positive margins, we don’t have the money to address social determinants of health, but it’s important. We need other people to help us with that, like community partners or the state,” Jacobson said.
WHA is a proud sponsor of WHN’s luncheon series.

From left: WHN Editor Tim Stumm, Susan Turney, Cathy Jacobson, Peggy Troy
When asked what the biggest issue facing hospitals is right now, Jacobson replied simply “workforce, workforce, workforce.” She went on to explain that includes workforce shortages, the cost of workforce, and the inability to do anything about it.
“A lot of people in different industries are experiencing workforce shortages, but our workforce issues are different,” said Jacobson. “First of all, this workforce is battered and bruised from COVID. And second, other businesses have the ability to shut their doors when they don’t have workers, but we cannot do that. Our emergency rooms remain open 24/7,” she continued.
Turney agreed and elaborated on the scope of the health care workforce shortage. “Pre-pandemic, our workforce was already in crisis. We were already having difficulty with recruiting and retaining health care workers,” said Turney. “But it’s not just clinicians, but all positions within our facilities,” Turney added.
Troy added that remedying the problem will take time and maintaining the workforce pipeline, for all types of positions, is a tactic they are using for the long term. “It takes a long time to train a nurse, but we have other opportunities, too,” Troy said. “We need to teach younger kids about what health care is all about and the many different avenues in which they can work in a hospital.”
When it comes to financial pressures, Jacobson said while inflation is a factor, she called out utilization as the main driver. She explained there are two things happening – patients coming into the hospital are sicker, and patients are boarded in the hospital who do not need to be due to inadequate discharge placement. Both of these require more staff and more resources, adding to the cost of care.
Jacobson said, “This is clearly exacerbating all the issues we are having right now. We are working with our colleagues from the Wisconsin Hospital Association to try to get money to the right parts of the system to open up capacity in the hospital.”
Troy added that emergency department visits at Children’s Wisconsin have tripled this year as they are dealing with a “tripledemic,” with a high volume of cases with respiratory illnesses, like RSV, flu and COVID. Turney shared that Marshfield Clinic has stood up their incident command to manage capacity issues.
“Beds are full, and we don’t have the staff. That means patients are sitting in emergency rooms and not getting the care they need,” Turney said.
“We haven’t raised our prices. If you are getting a double digital increase from your insurance company, that is not coming to your local hospital,” Jacobson said.
All three panelists agreed that changes are needed to address these problems, and they called on the state to help with investments in the health care workforce and easing regulatory barriers.
“We are not looking for a bailout. We need some help on the topline, like with retention bonus. The state can help us with that. Also, it should not take months to get someone credentialed and licensed to work in Wisconsin,” said Jacobson.
Troy emphasized the importance of addressing social determinants of health to help alleviate the high acuity of patients. Jacobson expressed concern for funding social determinants of health initiatives as hospital margins tighten and suggested partnering with the community in this space.
“When we don’t have positive margins, we don’t have the money to address social determinants of health, but it’s important. We need other people to help us with that, like community partners or the state,” Jacobson said.
WHA is a proud sponsor of WHN’s luncheon series.
Vol. 66, Issue 50
Thursday, December 15, 2022
Board Members Emphasize Workforce Concerns, Discuss Financial Pressures on Panel in Milwaukee
WHA board members participated as key speakers for the Wisconsin Health News (WHN) event on Dec. 13 held in Milwaukee. The panelists featured Cathy Jacobson, CEO, Froedtert Health; Peggy Troy, CEO, Children’s Wisconsin; and Dr. Sue Turney, CEO, Marshfield Clinic Health System. The panelists discussed top issues impacting their hospitals, including capacity and delayed discharge concerns and financial challenges, but all three health system leaders emphasized workforce as a main pressure point.

From left: WHN Editor Tim Stumm, Susan Turney, Cathy Jacobson, Peggy Troy
When asked what the biggest issue facing hospitals is right now, Jacobson replied simply “workforce, workforce, workforce.” She went on to explain that includes workforce shortages, the cost of workforce, and the inability to do anything about it.
“A lot of people in different industries are experiencing workforce shortages, but our workforce issues are different,” said Jacobson. “First of all, this workforce is battered and bruised from COVID. And second, other businesses have the ability to shut their doors when they don’t have workers, but we cannot do that. Our emergency rooms remain open 24/7,” she continued.
Turney agreed and elaborated on the scope of the health care workforce shortage. “Pre-pandemic, our workforce was already in crisis. We were already having difficulty with recruiting and retaining health care workers,” said Turney. “But it’s not just clinicians, but all positions within our facilities,” Turney added.
Troy added that remedying the problem will take time and maintaining the workforce pipeline, for all types of positions, is a tactic they are using for the long term. “It takes a long time to train a nurse, but we have other opportunities, too,” Troy said. “We need to teach younger kids about what health care is all about and the many different avenues in which they can work in a hospital.”
When it comes to financial pressures, Jacobson said while inflation is a factor, she called out utilization as the main driver. She explained there are two things happening – patients coming into the hospital are sicker, and patients are boarded in the hospital who do not need to be due to inadequate discharge placement. Both of these require more staff and more resources, adding to the cost of care.
Jacobson said, “This is clearly exacerbating all the issues we are having right now. We are working with our colleagues from the Wisconsin Hospital Association to try to get money to the right parts of the system to open up capacity in the hospital.”
Troy added that emergency department visits at Children’s Wisconsin have tripled this year as they are dealing with a “tripledemic,” with a high volume of cases with respiratory illnesses, like RSV, flu and COVID. Turney shared that Marshfield Clinic has stood up their incident command to manage capacity issues.
“Beds are full, and we don’t have the staff. That means patients are sitting in emergency rooms and not getting the care they need,” Turney said.
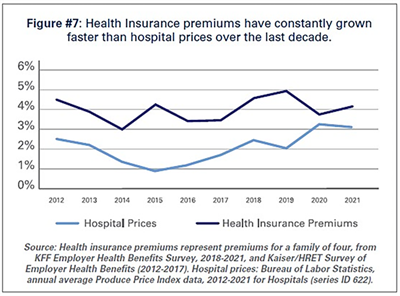 Both Turney and Jacobson noted a disconnect between what consumers pay in insurance premiums and what insurance companies pay hospitals for health care. As an American Hospital Association (AHA) report points out, hospital prices have grown an average 2.1% per year over the last decade, about half the average annual increase in health insurance premiums.
Both Turney and Jacobson noted a disconnect between what consumers pay in insurance premiums and what insurance companies pay hospitals for health care. As an American Hospital Association (AHA) report points out, hospital prices have grown an average 2.1% per year over the last decade, about half the average annual increase in health insurance premiums.
“We haven’t raised our prices. If you are getting a double digital increase from your insurance company, that is not coming to your local hospital,” Jacobson said.
All three panelists agreed that changes are needed to address these problems, and they called on the state to help with investments in the health care workforce and easing regulatory barriers.
“We are not looking for a bailout. We need some help on the topline, like with retention bonus. The state can help us with that. Also, it should not take months to get someone credentialed and licensed to work in Wisconsin,” said Jacobson.
Troy emphasized the importance of addressing social determinants of health to help alleviate the high acuity of patients. Jacobson expressed concern for funding social determinants of health initiatives as hospital margins tighten and suggested partnering with the community in this space.
“When we don’t have positive margins, we don’t have the money to address social determinants of health, but it’s important. We need other people to help us with that, like community partners or the state,” Jacobson said.
WHA is a proud sponsor of WHN’s luncheon series.

From left: WHN Editor Tim Stumm, Susan Turney, Cathy Jacobson, Peggy Troy
When asked what the biggest issue facing hospitals is right now, Jacobson replied simply “workforce, workforce, workforce.” She went on to explain that includes workforce shortages, the cost of workforce, and the inability to do anything about it.
“A lot of people in different industries are experiencing workforce shortages, but our workforce issues are different,” said Jacobson. “First of all, this workforce is battered and bruised from COVID. And second, other businesses have the ability to shut their doors when they don’t have workers, but we cannot do that. Our emergency rooms remain open 24/7,” she continued.
Turney agreed and elaborated on the scope of the health care workforce shortage. “Pre-pandemic, our workforce was already in crisis. We were already having difficulty with recruiting and retaining health care workers,” said Turney. “But it’s not just clinicians, but all positions within our facilities,” Turney added.
Troy added that remedying the problem will take time and maintaining the workforce pipeline, for all types of positions, is a tactic they are using for the long term. “It takes a long time to train a nurse, but we have other opportunities, too,” Troy said. “We need to teach younger kids about what health care is all about and the many different avenues in which they can work in a hospital.”
When it comes to financial pressures, Jacobson said while inflation is a factor, she called out utilization as the main driver. She explained there are two things happening – patients coming into the hospital are sicker, and patients are boarded in the hospital who do not need to be due to inadequate discharge placement. Both of these require more staff and more resources, adding to the cost of care.
Jacobson said, “This is clearly exacerbating all the issues we are having right now. We are working with our colleagues from the Wisconsin Hospital Association to try to get money to the right parts of the system to open up capacity in the hospital.”
Troy added that emergency department visits at Children’s Wisconsin have tripled this year as they are dealing with a “tripledemic,” with a high volume of cases with respiratory illnesses, like RSV, flu and COVID. Turney shared that Marshfield Clinic has stood up their incident command to manage capacity issues.
“Beds are full, and we don’t have the staff. That means patients are sitting in emergency rooms and not getting the care they need,” Turney said.
“We haven’t raised our prices. If you are getting a double digital increase from your insurance company, that is not coming to your local hospital,” Jacobson said.
All three panelists agreed that changes are needed to address these problems, and they called on the state to help with investments in the health care workforce and easing regulatory barriers.
“We are not looking for a bailout. We need some help on the topline, like with retention bonus. The state can help us with that. Also, it should not take months to get someone credentialed and licensed to work in Wisconsin,” said Jacobson.
Troy emphasized the importance of addressing social determinants of health to help alleviate the high acuity of patients. Jacobson expressed concern for funding social determinants of health initiatives as hospital margins tighten and suggested partnering with the community in this space.
“When we don’t have positive margins, we don’t have the money to address social determinants of health, but it’s important. We need other people to help us with that, like community partners or the state,” Jacobson said.
WHA is a proud sponsor of WHN’s luncheon series.
IN THIS ISSUE
- Registration Now Open for WHA 2023 Physician Leadership Development Conference
- Tell Your Story in the 2023 Wisconsin Health Care Workforce Report: Submit Stories by Jan. 16, 2023
- At Final Hearing, Legislative Council Study Committee on Occupational Licenses Advances WHA-Backed Legislation to Improve Health Care Licensure Process
- Advocate Health’s Nan Gardetto Receives WHA Trustee Award
- Board Members Emphasize Workforce Concerns, Discuss Financial Pressures on Panel in Milwaukee
- WHA Awarded AHW Seed Grant for Community-Based Initiative
- Congress Poised to Pass One-Week CR Extension, Including Funding for MDH and LVH Hospital Designations
- GUEST COLUMN: Health Care Staffing Shortages Make Big Impact on Liability and Workers’ Compensation Risks
- Webinar Recap: What’s Your Antibiotic Stewardship New Year’s Resolution?
- Social Care - Beyond Resources Webinar Recap

